frozen Shoulder

Frozen Shoulder
Frozen shoulder is a common diagnosis for shoulder pain. However, not every painful shoulder with limited movements is a frozen shoulder. Careful examination by an experienced Orthopaedic Surgeon is needed to rule out other causes. This video explains the frozen shoulder in Hindi language. you can get more details on this link.
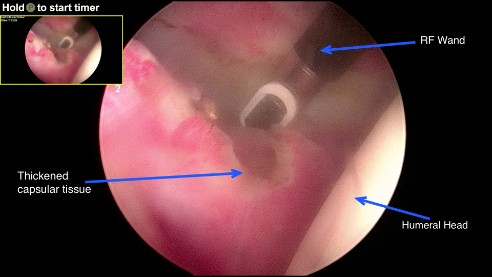
Frozen Shoulder released via Key Hole Surgery
The lateral picture represents release of the capsule whilst taking care to preserve the important structures like tendons, and cartilage.
Types
Many times the cause of a frozen shoulder may not be obvious. This is called idiopathic frozen shoulder. About half the patients have predisposing factors like diabetes, arthritis or may have had injury. Other relatively rare causes may include thyroid disorders, Parkinsonism, or heart conditions. They suffer from secondary frozen shoulder.
Pain can also arise from a variety of other causes like tendon tear, bursitis, or impingement. This can frequently get misdiagnosed as frozen shoulder.
Historically, three stages of frozen shoulder have been defined, although in reality, these are not distinct and overlap significantly:

Freezing (Painful) Stage
This is the acute inflammatory phase that is usually extremely painful. The symptoms in this stage that can last between 3-9 months.
Frozen (Stiff) Stage
This is when the acute pain settles down, but patients are left with varying degree of stiffness. The frozen stage can last 12 – 24 months in total.

Thawing (Resolution/ Return of Mobility) Stage
This is when tissues begin to loosen up, and movements begin to improve towards normal. Most patients however are left with slight deficit towards the end range. The stage can last another 12-18 months.
Overall, the natural cycle of frozen shoulder can last 2-4 years, there is considerable variation in individual presentation, and examination is important to establish the diagnosis.
It is a clinical diagnosis, but other investigations may be used to aid the diagnosis. Plain X-ray should be obtained to rule out arthritis, other investigations are rarely needed. Sometimes MRI scan may be necessary to rule out cuff tear or an occult fracture.
- Physiotherapy: Most patients benefit from physiotherapy input in the frozen or resolution stage.
- Hydrodistension: As explained by this patient, It is an outpatient procedure done under local anaesthesia. The success rate is 70-80% in suitable patients. If done at appropriate stage, most patients get excellent outcome from this procedure.
- Arthroscopic release: It involves releasing the thickened and tight capsule to restore the joint mobility. This is followed by early aggressive physiotherapy. The red inflamed tissue seen in the picture below is typical of adhesive capsulitis.
Here is a short video of the arthroscopic procedure. Please contact using the details on this website if you need a consultation.
A regional block with or without GA is used for the operation. The block is very useful for the first 24-48 hours when the pain is at its worst. Success rates after surgery vary between 80-95%.

